The musculoskeletal system includes: muscles, tendons, tendon sheathes, nerves, bursa, blood vessels, joints/spinal discs, and ligaments. MSDs may be caused or aggravated by the presence of one or any combination of the following risk factors: repetition, awkward or static postures, high forces, and contact stress. When these factors exist simultaneously, the risk of developing a MSD is significantly increased.
Research has found symptoms of discomfort for a dental team occurred in:
- Wrists/hands: 70%
- Neck: 70%
- Upper back: 68%
- Low back: 57%
- And shoulders: 60.0%
Most dental professionals (93% of those surveyed) had at least one job-related ache, pain, or discomfort in the 12 months prior to a survey carried out in 2008.
Conditions can vary from mild recurrent symptoms to severe and incapacitating. Early symptoms of MSDs include pain, swelling, tenderness, numbness, tingling sensation or loss of strength.
Factors Affecting Muscular-Skeletal-Nerve Disorders
- Static Postures
- Force: effort and pressure exerted
- Repetitive Movements: Frequency, Duration, Recovery Time
- Vibration
Injuries to the Body
Wrist
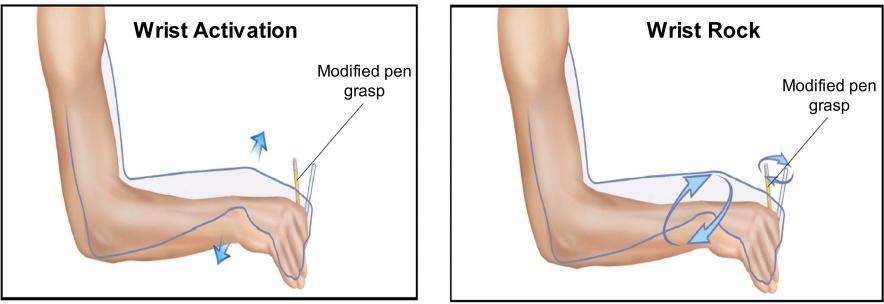
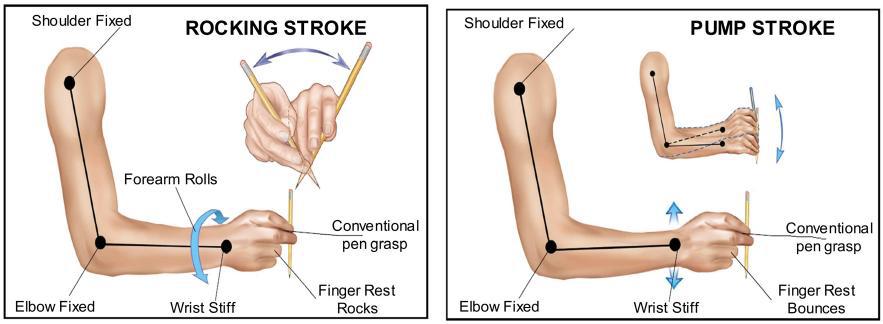
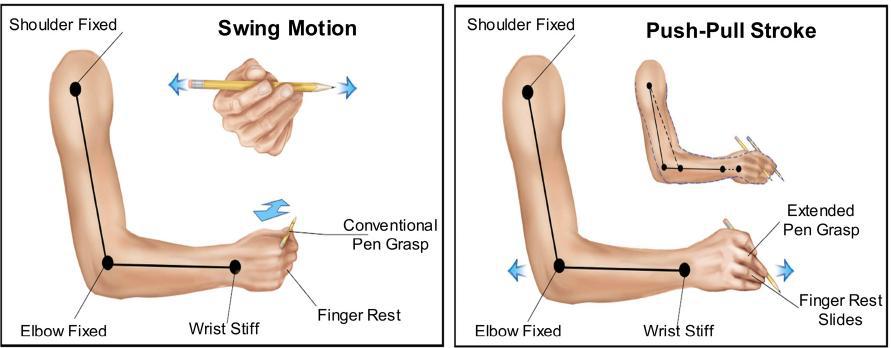
The risk factors associated with dental work that most commonly affect the wrists are chronic repetitive movements, awkward and static positions, mechanical stresses to digital nerves such as sustained grasps on instrument handles, extended use of vibratory instruments and inadequate work breaks. The wrist is in constant demand, often sustaining excessive and repeated stresses and strains. The safest position for the wrist is a straight or neutral position. Special care should be used to avoid bending the wrist downwards (flexion) or outwards (ulnar deviation).
- Carpal Tunnel Syndrome
- Tendonitis of the Wrist
- Guyon’s Syndrome
Fingers
- DeQuervain’s Tenosynovitis
Try to rest 2 fingers during dental work, this allows far less thumb pinch forces and reduction in muscle activity of the fingers, thumb, hand, and forearm. The closer one can position their finger rest to the target area, the greater the level of micro-control will be achieved.
Elbow
- Epicondylitis: either golfer’s (inside) or Tennis (outside)
- Cubital Tunnel Syndrome
Shoulders
- Bursitis
- Thoracic Outlet Syndrome
- Rotator Cuff Tear
- Rotator Cuff Tendonitis
Neck
Causes: Prolonged static neck flexion and shoulder abduction or flexion, lack of upper-extremity support, and inadequate work breaks. Awkward postures are often adopted to obtain better views of the intraoral cavity, provide a more comfortable position for the patient and to coordinate their position relative to the dentist or assistant.
- Myofascial Pain Disorder
- Cervical Spondylosis (Arthritis)
- Cervical Disc Issues
- Cervical Joint Disorders
Back
The main risk factors associated with dental work are the sustained awkward postures and poor seating. Most individuals with low back pain do not simply injure their back in one incident but rather gradually over time. Repeated stresses from over the years begin to add up and slowly cause degeneration of various parts of the spine, resulting in low back pain.
- Disc Problems: In a seated posture the pressure in the lumbar discs increases by 50% as compared to standing. Additionally, sitting in an unsupported posture can cause twice the amount of stress as compared to standing.
- Sciatica
Ergonomics for the Dental Team
Seating
Research findings indicate that dentists and dental hygienists who sit 80 to 100% of the day are at an increased risk of developing low back pain.
Seat specifications:
Width: Twenty-five percent wider than the total breadth of the buttocks is considered adequate for the majority. The front edge of the seat should taper off and away from the legs so as not to impede circulation and nerve supply to the leg.
Height: The seat should also be height adjustable. When the feet are resting flat on the floor the angle between the spine and the thighs should be 90 to 110 degrees. An angle less than 90º flattens the lumbar curve of the spine and an angle greater than 110º gives the feeling like you are slipping off the seat.
Arm Support: Controversial whether to use. If elbow rests are present, they should be positioned just below seated elbow height so that when the shoulders are not elevated when using the rests. How to sit: Your tops of thighs slightly down, and bottom of thighs parallel to the floor. Sit back in chair and do not lean forward. Tendency is to do this to be closer to the patient. Places undo stress on the lower back, neck and shoulders.
Patient Chair
When seating a patient, optimal results will be achieved when their oral cavity is positioned at a height equal to the seated height of the clinician’s heart. Positioning the oral cavity above heart level will limit vantage and increase the rate of shoulder fatigue. On the other hand, positioning the oral cavity below the recommended height will result in non-neutral working postures including over declination of the head, forward and/or lateral bending of the torso, and inability of the clinician to access free movement in the clock positions.
When the patient is properly positioned your shoulders, elbows, and wrists should be in a neutral position, meaning that:
- your upper arms are close to your body
- your elbow / forearm angle is close to 90º
- your wrists are in line with the forearm with no more than a 20-30º extension
Most often the patient is not reclined far enough back to see into the mouth properly and the tendency is to then lean forward to see their upper molars properly. Try to recline the patient to horizontal and make use of the foot pedal to take them even further down. Their feet are slightly higher than the position of the head. Allows the dental team to have the correct focal distance to see into the whole mouth, distance is between 17 and 19 inches. Now have to bring base of chair up as it is far too low. Should have it high enough that your forearms are just above horizontal (slightly raised) and also allows you then to get under the chair. Your shoulders are back and your head is above your torso. You should be at around 11 o’clock for working. When working the lower front teeth you may have to raise the chair up slightly.
When both dentist and hygienist: The hygienist’s left leg in line with the patient and their eyes are 6 to 8 inches higher than the dentist’s. This height allows hygienist to be able to see whole oral cavity without bending at the trunk to look in. The instrument table is on a 45 degree angle to allow for a greater amount of space and for the hygienist to be able to turn to obtain the instruments. Their right leg is anchored under the instrument table. The dental chair is narrow, 24 to 27 inches. The wider the dental chair the further away the hygienist.
Dental Team: Should not rotate and bend to do your work on a patient.
Ultrasonic Tools
While ultrasonic tools can serve to reduce prolonged pinch gripping, they do expose the clinician to hand-arm vibration. Research has been controversial regarding the relationship between the use of ultrasonic scalars and the development of musculoskeletal problems.
Cord Management
The added weight of cords can often influence the level of muscle fatigue experienced by a clinician. Additionally, coiled hoses can cause the hands and wrists to do more work if the coils have too much resistance to deformation. It is recommended that retractable or coiled hoses be avoided and replaced with a pliable hose which consists of a swivel mechanism in the barrel. The 360 degree swivel cords also provide increased flexibility for managing the cord. Positioning heavier cords over the arm or across an armrest can also be beneficial for reducing muscle strain
Mouth Mirror
If you are unable to visualize the operating site directly while maintaining a neutral posture, you must use a mirror to prevent awkward body positioning, specifically of the neck and back.
It is important to remember that a mirror should be held lightly and lowered into the mouth with the handle held not more than 45 degrees from the vertical plane.
Magnification
Surgical Loupes
Working Positions
Stretching
Frequent stretch breaks can prevent detrimental physiological changes that can develop while working in static or awkward postures. In an attempt to prevent injury from occurring to muscles, joints and nerves, dental professionals should allow for rest periods to replenish and nourish stressed structures. If breaks are too far apart, the rate of damage could exceed the rate of repair and eventually.
Stretching can serve to:
- increase blood flow to muscles
- increase the production of joint synovial fluid
- reduce the formation of trigger points
- maintain normal joint range of motion
- increase nutrient supply to vertebral disks
- create a relaxation response in the central nervous system
- warm up the muscle before beginning to work
- Identify tight structures that are prone to injury